What You Should Know About Osteoarthritis (OA)
Additional forms of arthritis:
The following are the main types of arthritis among the many that exist. To guide treatment and management in the correct direction, it is necessary to differentiate between the various types of arthritis.
Rheumatoid arthritis is an autoimmune disorder in which the body’s own tissue, in this case the joints, is attacked by autoantibodies. This involves multiple painful, swollen, and aching joints.
Psoriatic arthritis: This form of arthritis affects both the epidermis and the joints. Joints such as the elbow and knee, as well as the genital region, may develop scaly, raised regions of skin. This may be followed by arthritis symptoms.
Gout is characterized by joint pain and rigidity, most commonly affecting the big toe, and secondary deposition of uric acid crystals within the joint space.
The pathophysiology of osteoarthritis can be simply explained as an imbalance in the regenerative and degenerative processes of cartilage on a metabolic and biochemical level, which can be precipitated by a variety of factors including age, gender, joint use and trauma, and other causative agents. Environmental factors causing synovial joint stress, such as injury, misuse, and trauma, etc. Interaction with natural predisposing factors, such as gender and age, to induce the onset of the pathology.
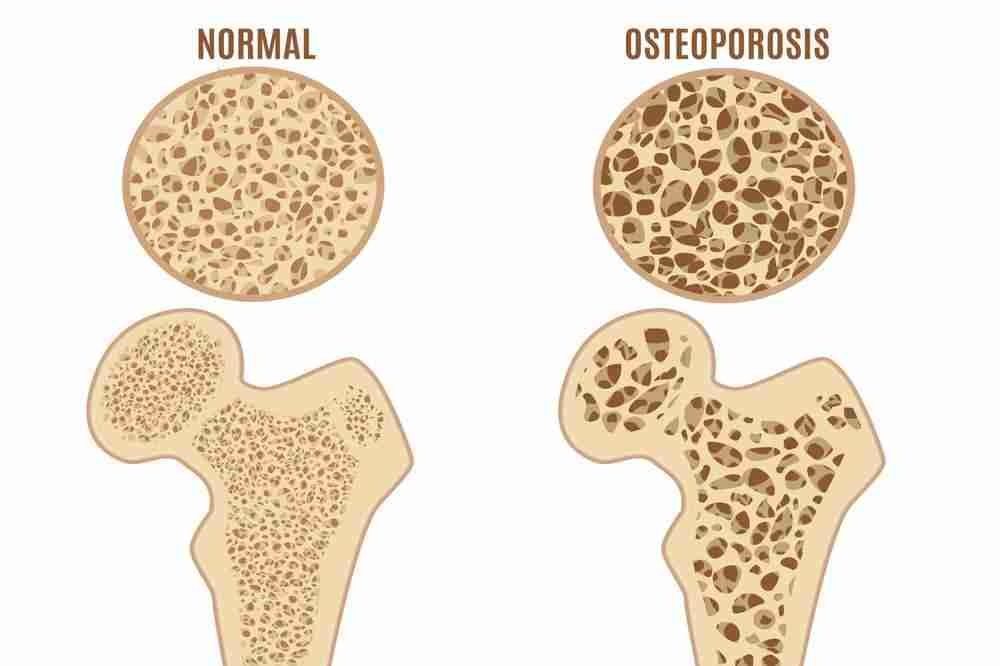
Normal cartilage degeneration versus osteoarthritis
Typically, degeneration induces the replacement of old cartilage cells with new ones. In OA, which is characterized by inflammatory alterations, there is a release of metalloproteinase MMPs and other inflammatory cytokines. Under the influence of these compounds, the number of chondrocytes, or cartilage cells, increases initially. Inflammation is always accompanied by the production of enzymes that result in cartilage dissolution. In OA, these degenerative changes, which are typically accompanied by regenerative processes, result in cartilage loss at the bone extremities. Similar degenerative alterations are also observed in bone tissue. However, the exact mechanism by which these cytokines are initiated remains speculative. One theory implies that the number of receptors on the joint surfaces that respond to these chemicals has increased.
The repercussions of cartilage loss
The cartilage at the bone extremities functions as a shock absorber. It is composed of elastic fibers that permit the joint’s full range of motion. Without this lubricating surface, there is a great deal of friction between the adjacent bones at the joint. This causes the bone, which was beneath the cartilage, to experience progressive sclerosis. This is also accompanied by the development of cysts at the bone extremities. These cysts cause the bone end to become disproportionately thickened and deformed. When in motion, the tendons and ligaments attached to the bone ends produce excessive stress on the bones, which explains symptoms such as pain and stiffness. The result is bone fusion and loss of joint space at the affected joint. Initially, cell loss stimulates the production of new bone cells. However, this new bony outgrowth is irregular and settles around the joint, causing osteophytes to form. Due to the progressive loss of cartilage, the symptoms may persist throughout the duration of the process, which may take decades.
There are chemical factors that counteract the effect of inflammatory cytokines by stimulating the synthesis of chondrocytes, thereby balancing the regenerative process. In osteoarthritis, this equilibrium is tipped in favor of degeneration. These modifications differ from those of aging cartilage. OA is distinguished by differences in the water content, activity of degrading enzymes, and concentration of specific degraded type2 collagen fibers in aging and osteoarthritis-affected collagen. New research may provide additional insight into the pathology, allowing for the development of more effective treatment plans.
