Pathology and physiology
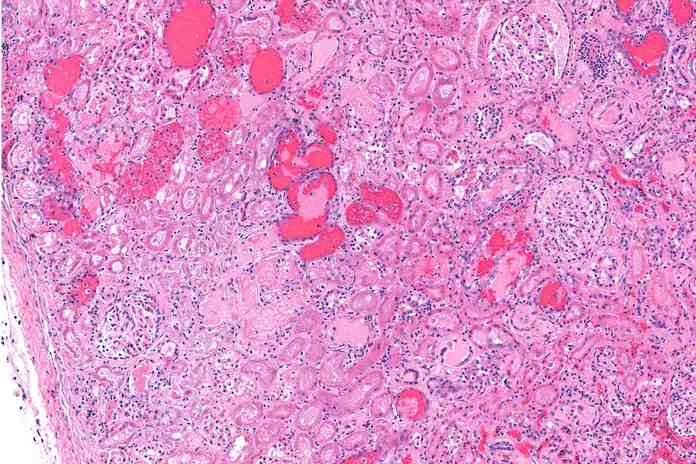
Hemolytic uremic syndrome (HUS) is a potentially fatal condition characterized by the elimination of red blood cells and renal failure. HUS is more prevalent in children than in adults, with a highest incidence between ages 4 and 10. Certain strains of E. coli bacteria cause a blood infection that leads to this condition. This bacteria then assaults the lining of the child’s small intestine, resulting in a “leakage” of various cells into the bloodstream. If the bowel infection becomes severe, abnormalities in the production of their membrane proteins can contribute to the formation of red blood cells. The composition of urine will then begin to diminish until it is a very dark red or even maroon hue.(3)
It is caused by the elimination of red blood cells and platelets by the immune system, as well as thrombocytopenia. The patient has internal hemorrhaging, renal insufficiency, and neurological impairment. The patient may eventually develop acute renal failure, resulting to death.
HUS may also be caused by contaminants in food or water, the use of certain medications such as steroids and cancer chemotherapy, exposure to monoclonal antibodies and molecularly cloned human proteins, and autoimmune disorders. Ten to twenty times more frequently than in elder children and adults, HUS occurs in children under the age of five. In the majority of cases, it is self-limiting, and full recovery occurs within two weeks to six months. The population most at risk for developing HUS is infants younger than 5 years old and of western European descent. There are two major complications that can result in mortality if they develop: circulatory collapse and acute kidney failure. The global mortality rate approaches 10%.
