Tennis elbow affects your muscles and tendons. Tennis elbow is caused by the repetitive use of your arms. Overuse of the arm is a common cause. It’s more common among people who play sports like tennis. This can be caused by everyday tasks such as carrying groceries or using a screwdriver.
Tennis elbow can cause stiffness and pain in your hand and arm. Tennis elbow can be treated by resting your arm and taking over-the-counter pain medications. Ice the area that is injured to relieve pain. It usually goes away on its own after a few months or weeks. You may need to consult a doctor if the pain persists.
You can take steps to ease pain and accelerate healing. If needed, rest your arm, apply ice to it and take pain medications over-the-counter. Exercises can be done to strengthen and stretch your muscles and tendons.
Pathophysiology
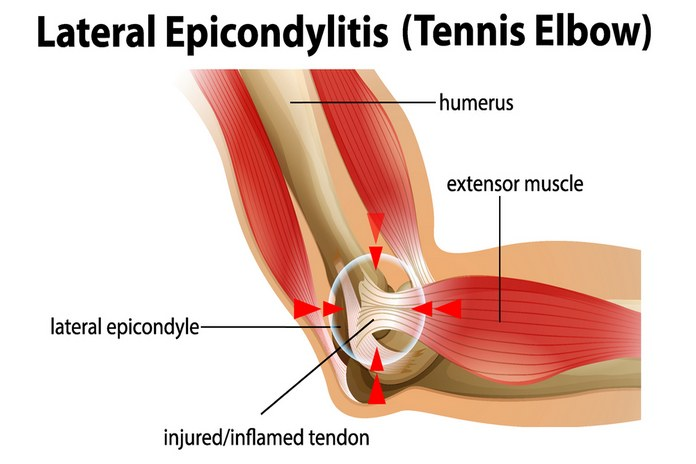
Tennis elbow’s pathophysiology is unknown. However, it is thought that the disease is caused by a micro-trauma to the extensor tendons. Micro traumas can be caused from repetitive movements of the hand and arm, like when playing tennis. Tennis elbow can also be caused by typing or using a screwdriver. This condition affects more men than women, and is most common between 30 and 50 years old.
Tennis elbow can cause pain to increase on the outside elbow when you grip or lift objects. In addition, there may be tenderness and swelling in the affected area. In severe cases, the arm may have difficulty moving. A physical examination is used to diagnose the condition. X-rays are sometimes taken to rule out any other conditions.
A 2015 article discusses the multidimensionality of tennis elbow. LE is caused by changes to the cellular and matrix structures of tendon, as well as changes in nociceptive transmission and muscle function.
Tendon Dysfunction According to research, the cellular changes in the tendon are similar with those seen in other tendinopathies. Degenerative and reactive tendinopathies are now seen as one continuum. Tendon pain is no more viewed as a inflammatory process and tendinitis no longer serves as a diagnostic term. They discuss how tendons react to loads and how training can promote healing in regards to LE. However, they also discuss tendon matrix and cellular changes that lead to tendon dysfunction. Stress-deprivation has a number of effects on tendons, including increased fibroblasts and collagen that is not aligned longitudinally, as well as decreased stiffness and strength. To improve, we need to assess each patient and determine the correct level of loading on their tendons.
Changes in the pain system: A large body of recent research shows that complex central changes are occurring when tendinosis is treated. There is no condition that doesn’t have an effect on the pain system. This image sums up so much information about lateral epichondylalgia, and it is my favorite from the NOI group. According to Coombes Bisset Vicenzino 2008, “substance-P and calcitonin-related peptide (CRP) reactive nerve fibers” are located within the proximal ECRB tendons along with small vessels. These pain modulators are powerful! LE patients often experience cold hyperalgesia and lowered pain thresholds over the lateral epichondyle. Although thermal pain thresholds are not as common in LE patients, they still play a role when assessing complex cases. Motor impairments include reduced strength and changes to motor control.
Jill Cook and others who study tendon strength, strength of shoulder external rotation, and other tendon-related research focus on supination/pronation control. In terms of pathophysiology, LE is a multidimensional condition that involves three major components: the muscles involved, the tendon, and the central and local nervous systems.
