Spinal Stenosis: Pathophysiology
The pathophysiology behind spinal stenosis involves a combination of mechanical compression and degenerative instabilities that manifests as cord dysfunction. Spurs are caused by the degeneration and collapse of intervertebral discs with age. Mostly, this occurs between C5-6 andC6-7. This level displays a relative decrease of spinal motion. Levels C3-4, C4-5 and C5-6 show an increase. As a result of physiological stress, osteophytes form on the superior and inferior margins. As a result, osteophytes can form in two different ways – anterior or posterior. Posterior osteophytes can also cause lateral recess stenosis. This impingement can cause damage to the spinal cord and nerve roots. Hypertrophy and synovial cysts of the facet joint may be linked to arthritic degradation, which further compromises the integrity of the spinal canal and neural foramina. (2)
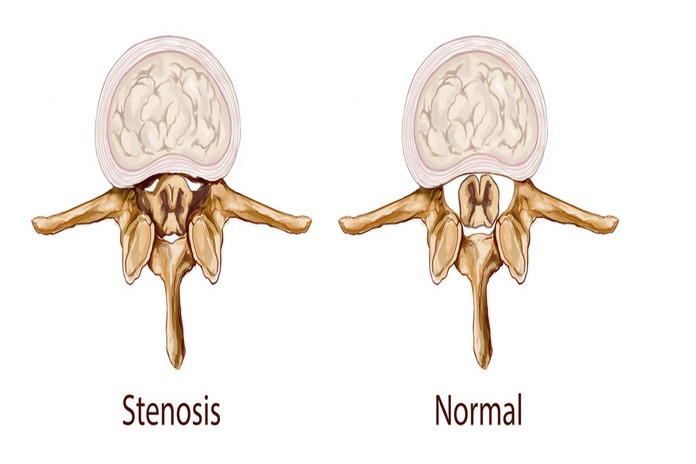
The central spinal canal narrows over time, causing a progressive stenosis of both the lateral recesses as well as the spinal canal. The spinal canal is primarily made up of the thecal sac and the dural membranes. The spinal canal can be narrowed by several factors without the need for surgery, infection, or tumors. They may include a hypertrophy at the uncovertebral joints in the neck or facet joints.
The cervical spine becomes instabile due to degeneration and abnormal movement, resulting in anterolisthesis or retrolisthesis. Listhesis compresses C3-4 and 4-5, while spur formation compresses C5-6 and 6-7. This is often accompanied by ligamentum flvum hypertrophy, which comprises the posterior canal.
The cord is further damaged by repeated dynamic injuries caused by normal neck movements. Static and dynamic compression forces are responsible for spinal cord injuries and myelopathy.
Degenerative disk disease and disk desiccation can cause segmental instability. As a result, the facet joints or vertebrae body hypertrophy. Hypertrophied IAPs in the cephalad spinal bodies can cause spinal canal stenosis. The HNP and the narrowing of disk space, as well as ligamentum flavum Hypertrophy, further reduce canal volume.
The superior articulating processes (SAPs) of the caudal verterbral body can also cause foraminal stenosis or lateral recess. Facet hypertrophy can impinge on the L4 nerve roots in the foramen, and the proximal sheaths of the L5 nerve roots may be affected by lateral recess hypertrophy. Most commonly, degenerative stenosis affects two lower motion segments: L3-L4, and L4-L5. There is a transition zone between the mobile sacrum and mobile lumbar spinal segment. The posterior joints are more susceptible to rotational stresses because of the lack of sagittal alignment in this area.
