Pulmonary Embolization Pathophysiology
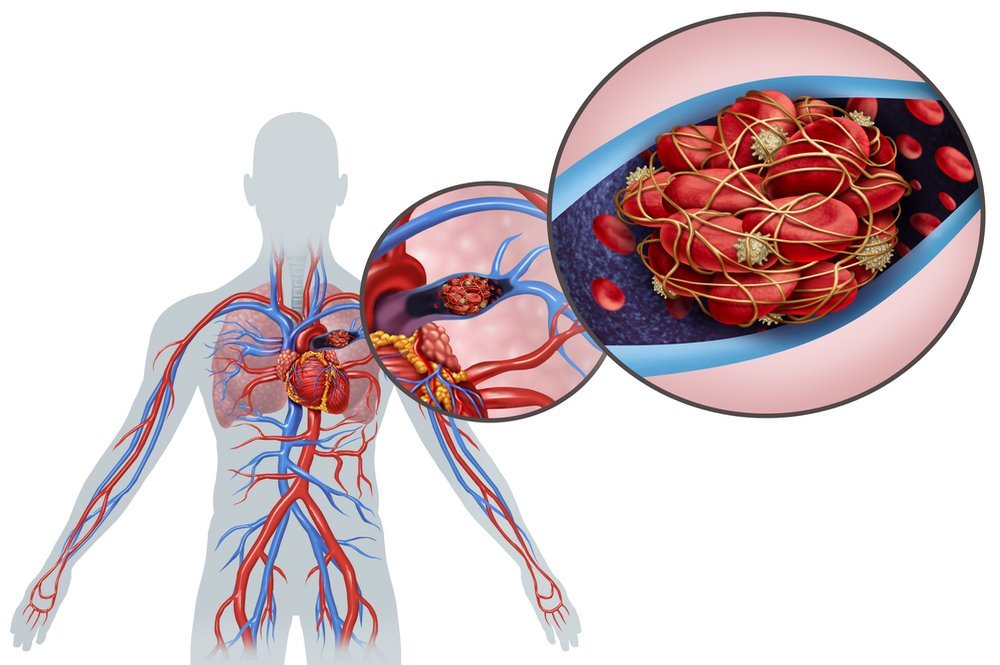
When blood clots from deep veins break off and begin to embolize in the pulmonary circulation, a pulmonary embolism occurs. Blood clots can cause vascular obstruction in the lungs, which affects blood circulation and gas exchanging. Lower lobes of the lungs are affected more often than upper lobes due to the more frequent involvement of bilateral lung tissue. The larger blood clots start to wedge in the main pulmonary arterial while the smaller blood clots are located the peripheral arteries. Smaller blood clots in the peripheral arteries lead to intra-alveolar death, resulting in pulmonary embolism. Nearly 10% of pulmonary embolism sufferers develop pulmonary infarction without having any cardio-pulmonary conditions. [7]
The alveoli require more space to ventilate than the capillaries in the lungs. The dead space ventilation contributes to the mismatch in ventilation-perfusion rate with vascular obstruction of the arteries and adds up to the pulmonary vascular resistance. The release of hormone mediators, such as serotonin and thromboxanes from activated platelets, may cause vasoconstriction even in areas free from pulmonary embolism. The right ventricle fails as the pulmonary arterial increases the systolic blood pressure. As the right ventricle fails, impairments in the left ventricle also develop.
Other than risks such as insufficient coronary filling, syncope or hypotension, sudden deaths, or electromechanical dissociation, rapid progression to myocardial ischaemia may occur. The high mortality and morbidity rate of pulmonary embolism can make it difficult to treat the condition early. As 30% of pulmonary embolism sufferers die before receiving treatment, there has been a failure to diagnose pulmonary embolism that requires serious management. Only 8% of patients who receive effective treatment survive to live a normal, healthy life. Unfortunately, pulmonary embolism can be asymptomatic or present in sudden death.
The symptoms and signs of pulmonary embolism, such as dyspnea and chest pain, tachycardia and shock, are also present in other conditions, including pneumonia, congestive cardiac failure and myocardial ischemia. In the prospective studies, pulmonary embolism patients with early diagnosis reported a wide variety of symptoms. Some of these symptoms were similar across all patients. Tachypnea, with a 54% percentage along with 24% of tachycardia, is one of the most common symptoms of pulmonary embolism. Dyspnea is the next most common symptom, which usually occurs within seconds after the onset of pulmonary embolism. There were also 34% of patients who had a cough and 41% with calf/thigh swelling. In comparison with the other symptoms, tachycardia was the most common symptom in only 24% of patients. These studies do not include critically ill patients who have kidney failure or higher creatinine values, as pulmonary embolisms develop differently in these cases.
