Common Osteoporosis Causes

Osteoporosis has multiple origins, which can be divided into primary and secondary causes. [3] These consist of:
Low calcium content
Calcium, which makes up approximately two-thirds of bone matrix, is by far the most essential factor in bone health. Adequate calcium intake early in life contributes to improved bone development, bone density, and bone health in the future.
Inadequate dietary intake: consuming a diet low in calcium during infancy and adolescence can negatively impact bone health later in life. Many females in underdeveloped and developing nations are predisposed to osteoporosis due to malnutrition.
Poor absorption: you may develop osteoporosis despite consuming a calcium-rich diet. This can be caused by an abnormal absorption of calcium from the intestine owing to a disease, a side effect of medication, or age-related physiologic changes. The calcium is then not assimilated, resulting in osteoporosis.
Lack of Vitamin D
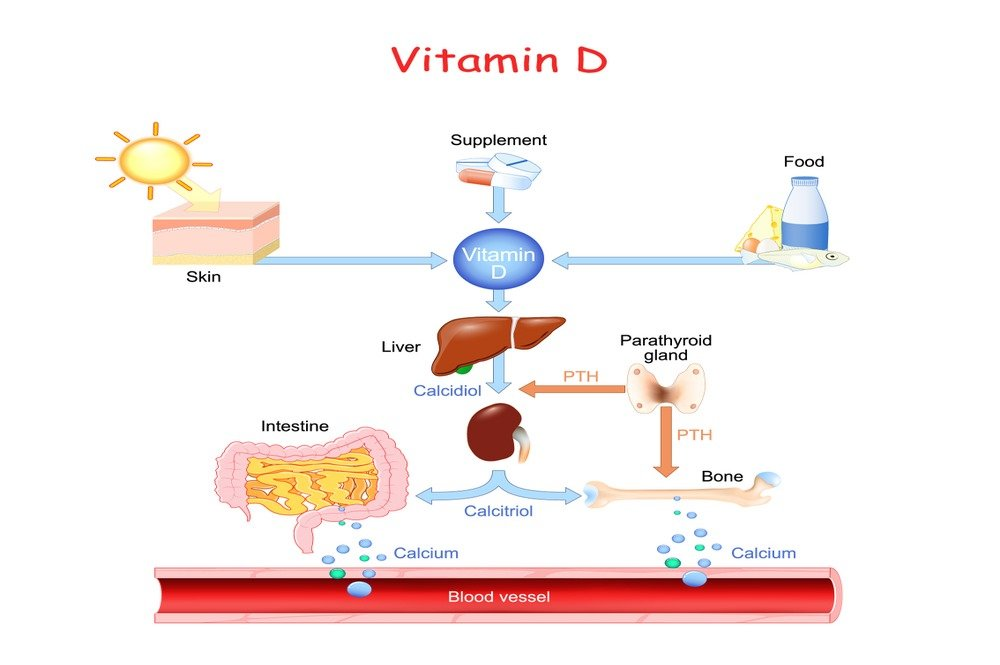
Vitamin D is essential for the intestinal absorption of dietary calcium. It also regulates the phosphate homeostasis in the body. It can also indirectly affect calcium levels by controlling the secretion of parathyroid hormone. Parathyroid hormone demineralizes bone in order to increase blood calcium levels.
Sun exposure allows the epidermis to produce vitamin D efficiently. It must undergo additional processing in the liver and kidneys to become the active form.
The senile form of osteoporosis is caused by a decrease in the body’s ability to synthesize this vitamin, which decreases with age. Vitamin D deficiency can affect calcium levels in the body, which can occur in bedridden patients and individuals with limited daytime exposure.
Endocrine Problems

Calcium levels must be maintained in both the circulation and the bones. Several hormones are actively and passively implicated in this homeostasis.
Estrogen is the female reproductive hormone, and it plays a role in bone growth during adolescence. It stimulates the bone-forming cells, or osteoblasts, to become active. In postmenopausal women, the progressive loss of this hormone favors osteoclastic or bone-resorption activity, resulting in porous bones.
Testosterone is the reproductive hormone for men. This hormone also declines with age in men, resulting in decreased bone mass and compromised bone density.
Thyroid hormones: the thyroid gland secretes an important calcium-regulating hormone called calcitonin. This hormone is responsible for the calcium-based mineralization of bone matrix. Any abnormality in the gland, such as a tumor or a change in the gland’s size, can therefore disrupt the calcium balance. Other thyroid hormones can also affect the metabolism of food elements and the general health of bones.
Parathyroid hormones: excessive secretion of this hormone, which can be caused by vitamin D deficiency or a parathyroid gland tumor, can induce osteoporosis by stimulating the activity of osteoclasts. The minerals of the bones are lost, and the calcium released from the bones accumulates in the blood.
Other hormones: the activity of steroid hormones secreted by the adrenal glands can also influence bone health by influencing the body’s overall metabolism.
Gastrointestinal Conditions
Despite a sufficient calcium intake, gastrointestinal diseases can decrease calcium absorption from the intestines.
Eating disorders, such as bulimia nervosa and anorexia, affect female adolescents and preteens. Due to the limited risk perception among elderly women, the associated osteoporosis may go undetected. Nonetheless, according to a study [4], 44% of chronic anorexic patients are at risk for osteoporotic bone fractures. Dietary components are flushed from the body as a result of a restricted diet and/or regurgitation, leaving the body with insufficient nutrients.
Surgical procedures that involve the resection of portions of the gastrointestinal tract may reduce the surface area available for absorption of dietary components.
It has been reported that 40% of patients with inflammatory bowel disease suffer from fragility fractures. In this scenario, steroid therapy, inflammation, and malnutrition are the primary factors that can compromise bone health.
Congenital Ailments

This disorder, osteogenesis imperfecta, is the result of a genetic mutation responsible for collagen type 1 protein. This protein is an essential component of bone matrix, as well as the sclera of the eyes and the epidermis. The disease manifests a variety of symptoms. Patients may have aberrant posture due to bone deformities.
This chromosomal disorder characterized by connective tissue malformations has been reported [5] to decrease bone mineral content (BMC).
This connective tissue disorder, Ehler Danlos syndrome, also contributes to decreased bone mineral density and an increased risk of fractures.
Medical treatments

The effect of drugs on bone health is progressive; prolonged use of such medications results in a greater mineral deficiency and bone density deficit.
Steroids are the primary cause of osteoporosis caused by drugs. Steroids used to treat chronic inflammatory diseases can have a long-lasting effect on bone health. Osteoporosis has been linked to steroid use by an estimated 30-50%. Multiple factors, including osteoblasts decline, decreased calcium absorption from the intestine, and negative feedback inhibition of the sex hormones, are thought to contribute to the pathogenesis of this associated disorder. To prevent this complicated adverse effect, calcium and vitamin D are added to steroid therapy.
Cancer medications such as methotrexate can disrupt the equilibrium between bone formation and resorption, resulting in a loss of bone mass.
In the treatment of epilepsy, phenytoin, carbamazepine, and phenobarbital are used as anticonvulsants. A study found significant bone loss in women taking these medications. These medications increase vitamin D’s metabolic rate, which may contribute to its inactivation and a calcium imbalance.
To regulate the reproductive cycle, progestin-based contraceptives, particularly medroxyprogesterone, can inhibit endogenous estrogen synthesis. Loss of estrogen’s beneficial effect on bone health, particularly in young women, may result in decreased bone mass and density with prolonged use.
Other medications, such as loop diuretics used to treat cardiac disease, can stimulate calcium excretion in the urine. Although the relationship between protracted heparin use and decreased bone mass is observed, its pathophysiological basis has not yet been elucidated.
