Why Hyperhidrosis Occurs
After infarction or hemorrhages in the cerebellum, failure in the cortical inhibitory centers of the brain can cause hyperhidrosis in addition to lesions. After spinal lesions, sweating may decrease to a certain degree or cease entirely, leading to the development of compensatory hyperhidrosis in the residual parts of the body. Most frequently, patients begin to experience the lack of seating in a manner that is less disruptive than the compensatory increase in perspiration. Nearly one to two percent of the population suffers from hyperhidrosis, in which the perspiration glands are no longer inhibited. (4)
The perspiration glands produce sweat regardless of the environmental conditions. Patients with hyperhidrosis, for instance, perspire even when seated, viewing television, or lying in air-conditioned rooms. Some patients also report to their physicians that they perspire profusely while swimming. Furthermore, the cause of hyperhidrosis depends on the variety of hyperhidrosis an individual has. Typically, excessive sweating is innocuous. In some instances, physicians do not know why a patient sweats excessively. On the other hand, hyperhidrosis may be caused by a medical condition that requires special attention. (5)
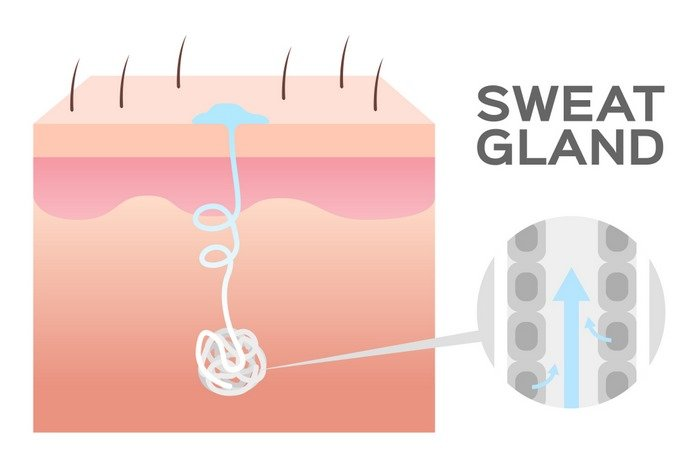
Sweating is the body’s natural cooling mechanism and a normal process for maintaining constant homeostasis to support all essential functions. When the body temperature begins to rise, the nervous system automatically sends a signal to the perspiration glands. In addition, as a result of anxiousness or anxiety, sweating typically occurs on the palms. The researchers distinguish the causes of each variety of hyperhidrosis, and the following is a description of the causes for both types:
Essential hyperhidrosis
Primary or focal hyperhidrosis is the form of excessive perspiration or hyperhidrosis that occurs most frequently. In the primary or focal form of hyperhidrosis, the nerves are typically responsible for sending hyperactive signals to the sweat glands. Despite the fact that the perspiration glands are not activated by any physical exertion or activity that causes an increase in body temperature. In addition, anxiety and/or tension exacerbate the problem of excessive perspiration. In addition to the face, the primary or focal form of hyperhidrosis typically affects the soles and palms.
It is commonly believed that primary or focal hyperhidrosis is caused by defective genes that run in families. The actual cause of primary hyperhidrosis is unclear, but those with a family history of hyperhidrosis are more likely to develop the condition themselves. A common factor in the underreporting or underdiagnosis of hyperhidrosis is the fact that many individuals with the condition never discuss excessive perspiration out of embarrassment. If hyperhidrosis appears to be prevalent among a large number of family members, it may be beneficial for researchers to gain a greater understanding of the causes and causes of hyperhidrosis.
For the purpose of determining the underlying cause of hyperhidrosis, the doctor first asks each patient about his or her symptoms. If you have focal visible excessive sweating for at least six months without any apparent cause, your doctor will determine whether you satisfy the following two criteria.
The perspiration is bilateral and relatively symmetrical (you perspire nearly equally on both sides of the body).
Normal activities are impeded by excessive perspiration.
The advent of excessive sweating occurred prior to the age of 25.
At least one episode of excessive perspiration per week is occurring.
You stop perspiring upon falling slumber.
Similar perspiration issues affect other members of your family as well.
If you satisfy at least two of the aforementioned criteria, there is a possibility that you have primary or focal hyperhidrosis. After a hyperhidrosis diagnosis has been confirmed, you must schedule an appointment with a healthcare provider who is familiar with the available treatment options. The medical pathophysiology underlying the primary variety of hyperhidrosis is nonexistent. Rather, it may be the result of a mutation that is passed from generation to generation.
There is an activation of certain nerves in the sweat glands when you sense your body overheating, when you are experiencing an emotional state or hormonal imbalance, or when you are moving your body vigorously. When these receptors overreact, excessive sweating results. For example, a person may only need to imagine a circumstance that causes anxiety in order to sweat profusely. The primary cause of hyperhidrosis is an overactive thermoregulatory center in the hypothalamus. The overactivity of the hypothalamic thermoregulatory center in the brain transmits nerve impulses to the eccrine perspiration glands via the sympathetic nervous system.
Some causes of primary hyperhidrosis episodes include:
Physical exercise
Spicy dishes
Stress Fever
warm weather
People used to believe that primary hyperhidrosis was related to a patient’s mental and emotional state. It was once believed that hyperhidrosis was a strictly psychological condition, affecting only those afflicted with stress, anxiety, or nervousness. Studies indicate that genetic mutations play a significant role in the development of hyperhidrosis, making it more likely to be an inherited disorder. The majority of patients with the primary form of hyperhidrosis have a parent or sibling with the disorder.
If a person’s sweat glands are always active, even in the absence of triggers or stimuli for perspiration, they should be evaluated for primary hyperhidrosis. People affected by primary hyperhidrosis typically produce perspiration from eccrine sweat glands. The majority of the body’s 2 to 4 million perspiration glands are eccrine sweat glands. There are abundant eccrine perspiration glands on the face, armpits, palms, and soles of the feet.
