Histological markers of cellulite
Other cellulite indicators are not visible on the surface of the skin, but may exist subcutaneously. Several distinct metabolic and physiological mechanisms are known to contribute to the histopathology of cellulite. These signs occur in sequence.
Fat deposition is not strictly related to cellulite, but it is a contributing factor. Particularly within adipocytes that resemble bubbles, women’s fat deposits at specific sites and in a specific manner.
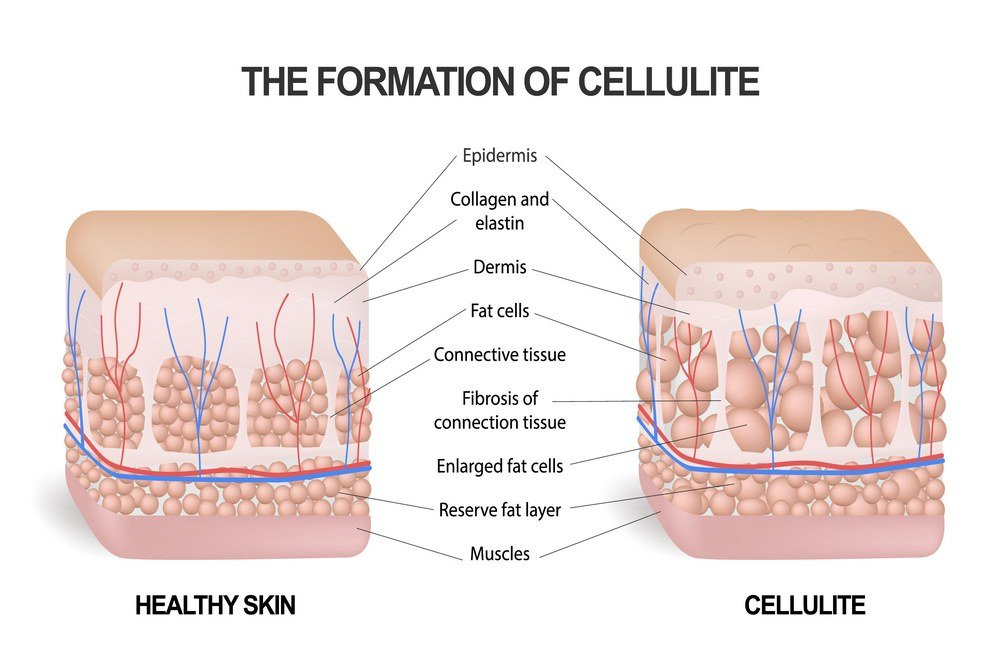
Variations in the matrix of connective tissue:It contains collagen and elastin filaments that provide flexibility and strength to the matrix. The proliferation of these fibers within cellulite tissues alters the tissue architecture.
Changes to the lymphatic system: The examination of ultrastructure biopsies reveals that the affected region undergoes lymphatic system remodeling. The edema pressure modifies the system of vessels that return excess fluid that has leaked through the blood vessels back into circulation. This system’s obstruction also appears to be responsible for the development of cellulite.
Remodeling of Microcirculation: The edema at the site of cellulite causes microvasculature congestion. This constriction of the blood vessels reduces blood flow to the affected area. Infrared imaging reveals this as a decrease in temperature in the local region.
Changes in interstitial fluid: The fluid that leaks from the microscopic capillaries accumulates in the intercellular spaces. According to microscopic investigations, cellulite tissue contains a higher proportion of protein in this fluid. Additionally, increased fluid pressure is recorded.
Cellulite is also known as Adiposis edematosa, or edematous adipose tissue. A increased concentration of glycosaminoglycan has been detected. As members of the biomolecule family known as mucopolysaccharides, they have a tendency to attract water. This localized water retention results in a distended appearance and microscopically detectable edema.
Inflammation: According to some research, inflammatory cells and other inflammatory alterations were detected at the site. This supports the theory that cellulite is caused by a moderate chronic inflammatory process. It has not yet been declared a definitive presentation, however.
Histopathology allows for a more thorough investigation of these symptoms. As demonstrated by ongoing research on the subject, there is a considerable remodeling of the fat cells that compose the subcutaneous fat layer as well as the collagen and connective tissue fibers that serve as a cage to contain this fat layer. These fibers separate the fat layer into segments composed of globules of fat cells and pull the epidermis between these segments. This causes the epidermis to develop characteristic bumps. On the same histopathologic principles, cellulite differs from simple obesity. Obesity is characterized by an increase in the size and number of adipocytes, cells that accumulate fat. However, a different mechanism is responsible for the distinctive topography of epidermis in cellulite. Cellulite is characterized by excessive fat accumulation in lobules, which manifests as bumps, and dense fibrous septa adhering to the skin and pulling it inwards, which manifests as depressions.
